Recommendations on impetigo and ecthyma
- Culturing the exudates is helpful, but treatment can be done without culturing.
- Impetigo: oral/topical abx; if outbreaks/numerous lesions oral form is preferred.
– Topical muciprocin or retapamulin bid for 5 days
- Ecthyma: oral is preferred.
- Oral therapy for impetigo and ecthyma is dicloxacillin/cephalexin for 1 week (normally MSSA). if MRSA, doxycycline/clindamycin/TMP-SMX.
Recommendations for purulent skin infections
- Treatment without culture is reasonable.
- Culture & stain from inflamed epidermoid cysts are not recommended.
– Inflammation and purulence are a reaction to cyst wall rupture and contains skin flora.
- I &D is the recommended treatment.
- Abx only in the presence of SIRS criteria. Abx should cover MRSA.
Recommendations for recurrent skin abscesses
- Look for local causes eg hidradenitis suppurativa, pilonidal cyst etc.
- If begin in childhood, the adult should be evaluated for neutrophil disorders,
- Should be drained and cultured. Treat with 5-10 days abx against the pathogen isolated.
- Consider a 5 day decolonization regimen bid of intranasal muciprocin, daily chlorrhexidine washed and decontamination of personal items. (weak evidence)
Recommendations for cellulitis and erysipelas
- Cultures are not routinely needed, unless malignancy on chemo, neutropenia or other forms of immunodeficiency.
- Typical cellulitis: oral abx against Streptococci. MRSA is unusual cause.
- Cover for MRSA and streptococci if the cellulitis is associated with penetrating trauma, IVDU, purulent drainage, MRSA infection evidence elsewhere, or SIRS (severe non purulent).
- Chck the interdigital toe spaces as treating fissuring or maceration may eradicate colonization with pathogens.
- Treatment duration is 5-10 days. Elevation of the affected limb is recommended.
- Weak evidence supporting use of systemic corticosteroids in non diabetic adult patient with cellulitis. Clinician must ensures NF is absent.
Recommendations for recurrent cellulitis
- Identify predisposing conditions eg venous insufficiency or toe web abnormality.
- Weak evidence supporting prophylactic abx (eg oral penicillin for 4-52 weeks or IM benzathine penicillin every 2-4 weeks) in patients with 3-4 episodes of cellulitis per year.
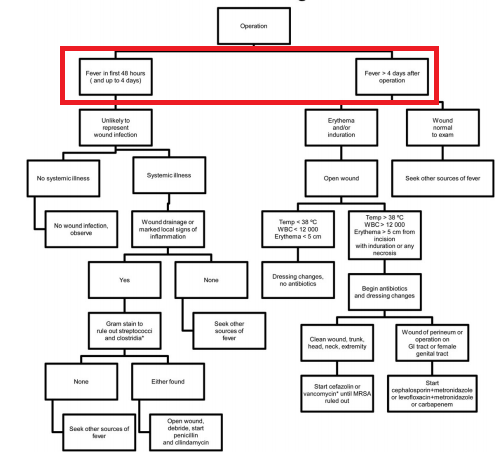
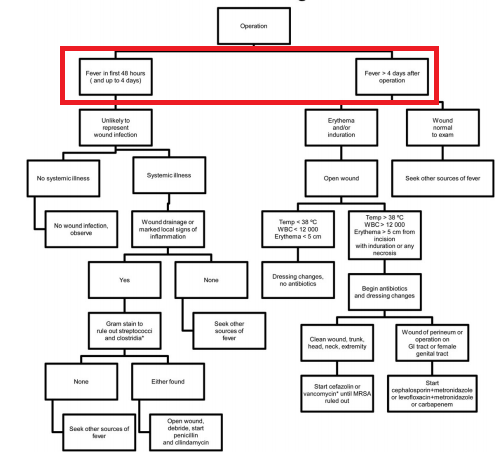
Recommendations for surgical site infections
- Suture removal + incision and drainage is most important therapy.
- Only give abx if there are systemic symptoms.
- Cover for MRSA if there are RFs eg recent abx/hospitalization or prior MRSA infection.
- Cover G- and anaerobes in GI and GU infections (cephalosporin/FQ + metronidazole).
Recommendations for NF
- Prompt surg.consultation.
- Broad empiric abx as the etiology can be polymicrobial eg vanco + zosyn or + ceftriaxone/FQ & metronidazole or + carbapanem)
- For documented Strep.A NF, penicillin + clindamycin is recommended.
** Consider NF if
- Pain out of proportion, edema and tenderness extending beyond the erythema
- Systemic intoxication
- Failure to respond to initial abx
- Presence of crepitus, bullous lesions or skin necrosis.
Most with NF should return to OR 24-36 hours after first debridement and daily thereafter until surgical team finds no further need for debridement. These wounds can discharge copious amount of fluid so aggressive fluid therapy is needed. Abx is continued until no further debridement is needed or patients improve clinically.
Recommendations for pyomyositis
- MRI is the recommended imaging modality.
- Culture should be obtained from the abscess material and blood (only 5-30% of blood culture will be positive).** Serum CK can be normal.
- Vancomycin is recommended for initial empirical therapy. Add abx that covers for G- bacilli in open trauma/immunodeficient patients.
- Like purulent skin lesions, drainage should be performed early.
- Repeat MRI if there is persistent bacteremia (identify undrained foci)
- For MSSA infection, use cefazolin or antistaphy penicillin.
Recommendations for gas gangrene
- Urgent surgical debridement.
- broad spectrum empiric therapy in the absence of definitive etiology.
- HBO therapy is NOT recommended as it has not been proven as a benefit to the patient.
Recommendations for animal and human bite wounds
- Prophylactic abx only for high risk wounds eg immununocompromised, asplenia, adv.liver disease, mod-severe injuries, especially to hands & face.
- PEP for rabies maybe indicated.
- Cover for both aerobic and anaerobic pathogens eg augmentin or cefuroxime or other 2nd & 3rd gen cephalosporin + clindamycin/metronidazole
** Other options: SMX-TMP/FQ + clinda/metro
** Do not use macrolides due to variable activity against P.multocida and fusobacteria.
- Give tetanus toxoid in patients without vaccination within 10 years.
- Do not perform primary closure on wounds except face (weak evidence).
Recommendations for immunocompromised patients
- Consider other ddx eg Sweet’s syndrome, GVHD, leucocytoclastic vasculitis. Always perform biopsy/aspiration to obtain material for histological and microbiological evaluation.
- Determine whether the current fever & neutropenia is recent, persistent (after 4-7 days) or recurrent.
- Risk stratify the patients. High risk = prolonged (>7 days) neutropenia (ANC < 100 cells/uL) or with MASCC score <21.
- For initial fever + enutropenia: vancomycin + antipseudomonal abx eg zosyn, cefepime is recommended. Duration of tx 1-2 weeks.
** For low risk patients, augmentin + ciprofloxacin can be used.
** levofloxacin has better G= coverage but less potent against P.aeruginosa than cirpofloxacin.
- CSF therapy should not be routinely used.
- For recurrent/persistent fever and neutropenia: yeasts and molds are the main cause.
– Candida: echinocandins for 2 weeks, lipid formulation amphotericin B with fluconazole is acceptable alternative
– Aspergillus: voriconazole or lipid formulation amphotericin B/posaconazole/echinocandins for 6-12 weeks.
– Mucor: amphotericin B or posaconazole
– Fusarium: voriconazole or posaconazole
– Also if suspect HSV/VZV, add IV aciclovir.
- Sens of single serum fungal antigen test eg (galactomannan or 1,2 B-D glucan) is low.
Other organism-specific recommendations
- Cat scratch disease: azithromycin
- Erysipeloid: penicillin or amoxicillin for 7-1 days
- B.mallei (aerobic, gram negative): ceftazidime, gentamicin, doxycycline, ciprofloxacin or imipenem based on in vitro efficacy.
** Known as glanders: ulcerating nodular lesions caused by B.mallei, humans because accidental host by inhalation of contact with horses/mules

5 take home messages
- Routine cultures of blood and tissues is not recommended for skin infections, except with systemic signs, immunosupression, malignancy or animal bites.
** In animal bites, blood culture only when there is systemic signs.
(http://emedicine.medscape.com/article/881171-treatment)
- For abscess, if no systemic signs, no abx is indicated.
- CA-MRSA is very unlikely in typical cellulitis, so in typical cellulitis only Streptococci coverage is needed. This is in contrast in purulent infection (empirical should cover CA-MRSA).
- Cover for MRSA if the cellulitis is associated with penetrating trauma, purulent discharge, IVDU or evidence of MRSA infections elsewhere. In surgical site infection, cover for MRSA if there is recent exposure eg prior hospitalization/abx use or history of MRSA infxn.
- Examine inter-digital toe spaces for fissuring/maceration. Abx treatment can reduce colonization.
5(+2) abx therapy to remember:
- Impetigo: topical muciprocin or retapamulin OR oral cephalexin/dicloxacillin; ecthyma: oral cephalexin/dicloxacillin
** If MRSA: doxycycline/clinda/TMP-SMX
- Cellulitis:
– Mild-moderate: penicillin or cephalosporin (PO in mild, IV in mod)
– Severe: vanco + Zosyn or carbapenem
- Surgical site infection
– Not GI/GU: cefazolin or vancomycin if MRSA is suspected
– GI/GU: 3rd gen cephalosporin/FQ + metronidazole (G- & anaerobes)
- NF or gas gangrene: vanco + broad spectrum eg Zosyn/carbapenem
- Animal bites: augmentin or 2nd or 3rd gen cephalosporin + metronidazole/clindamycin
** DO NOT use azithromycin

- Pyomyositis: Vanco, if immunocompromised/open trauma add gram negative coverage
- Immunocompromised (need to cover MRSA + PSA + fungal/viral etc)
– Mild: cipro (for P.aeruginosa) + augmentin
– Severe: vanco + Zosyn/cefepime/carbapenems
– Persistent/recurrent: add antifungals/antivirals
Reference:
Practice Guidelines for the Diagnosis and Management of Skin and Soft Tissue Infections: 2014 Update by the Infectious Diseases Society of America.




 Note that patient should keep finger in extension for 6 weeks.
Note that patient should keep finger in extension for 6 weeks.